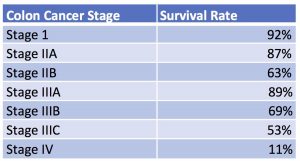
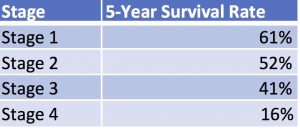
Men have more options than ever before when choosing a course of treatment, including a promising form of radiation therapy commonly known as proton therapy for prostate cancer (UF Health). 161,360 new cases of prostate cancer will be diagnosed in the U.S. in 2017, with an estimated 1 in 7 American men facing a diagnoses in their lifetimes. Those statistics may sound scary, but there are plenty of reasons to have hope if you or someone you love is fighting prostate cancer. As the ACA notes, survival rates for prostate cancer are quite high, and most American men diagnosed with this type of cancer do not die from it ([1] American Cancer Society).
Proton therapy (also called “proton beam radiation”) is a targeted method of treatment that provides a more accurate (and less toxic) alternative to conventional X-ray radiation. This therapy has been approved in the U.S. since 1988, but limitations in cost and infrastructure have limited its widespread use until somewhat recently (UF Health). If the idea of proton therapy is news to you, you may wish to learn more about it and ask your doctor if it might be a worthwhile addition to your treatment.
WHAT IS PROTON THERAPY?
Proton beam radiation is a method of targeting cancer cells with a focused dose of proton particles, attacking malignant cells with reduced exposure and damage to surrounding tissues and organs. This precise method of delivery permits doctors to use higher doses of radiation with fewer risks and side-effects for their patients. The greater accuracy allowed by proton therapy makes it a natural choice for treating tumors in delicate or otherwise difficult-to-target parts of the body, such as the brain or prostate (the latter of which is located in close proximity to the bladder, rectum, and reproductive organs). The low incidence of side-effects associated with proton therapy also means it is an excellent choice for treating certain pediatric cancers. Localized cancers – that is, cancers that haven’t metastasized, or spread to other parts of the body – are ideal candidates for treatment with proton therapy (UF Health).
So, how exactly does proton therapy work? In traditional X-ray radiation, doctors aim a beam of photons at a tumor in order to attack the malignant cells. But these X-rays don’t just stop short once they reach the tumor: they continue to pass through the body, leaving a kind of “exit wound” of damaged tissue on the way out. But protons are different: because of the way these heavy particles behave, doctors are able to aim a proton beam with just the right amount of energy to penetrate a tumor but stop short before exiting the body. This targeted approach helps reduce damage to healthy tissues and vital organs. ([1] UpToDate).
Proton radiation techniques continue to improve with new developments in technology. For example, some facilities now offer a type of proton therapy called “pencil beam scanning,” which is an even more precise method of delivering radiation to a tumor in subtle, brush-like strokes using a single proton beam (MD Anderson).
Researchers are also investigating what role other heavy particles (such as neutrons and carbon ions) might play in radiation therapy, though our clinical experience with them is still quite limited ([1] UpToDate). Proton therapy for prostate cancer (and other cancers) remains the most common form of heavy-particle therapy in use today (Journal of Clinical Oncology).
PROTON THERAPY FOR PROSTATE CANCER: WHAT ARE THE BENEFITS?
Proton radiation therapy is non-invasive, painless, and requires no recovery time following treatment. This is promising news for patients, who are able to pursue an advanced, effective treatment plan with minimal impact on their daily lives.
Prostate cancer patients typically receive daily proton treatments five days a week over a course of eight weeks; these treatments are administered on an outpatient basis, and often take no more than 15 to 20 minutes each day. In addition, prostate cancer patients who are treated with proton therapy experience minimal risk of impotence or sexual side-effects both during and after treatment (MD Anderson). Some patients experience mild fatigue, in addition to redness or hair loss around the direct treatment area, but other side effects on the whole appear to be minimal (Mayo Clinic).
Studies suggest that clinical outcomes for patients with proton therapy are similar to those treated with traditional X-ray radiation, which makes it an appealing option for many men who hope to maintain a higher quality of life during treatment without hindering their chances for a successful outcome ([2] UpToDate).
Proton therapy for prostate cancer is an FDA-approved treatment and is not considered to be an experimental therapy – that means you don’t have to be accepted into a study in order to get it. Cost is often a limiting factor, but more insurance plans are beginning to cover treatments as more facilities nationwide continue to adopt proton technology; the MD Anderson Cancer Center in Texas, the Mayo Clinic in Minnesota and Arizona, and the University of Florida Health Proton Therapy Institute are just some of the locations around the U.S. currently offering proton beam radiation to their patients. That said, widespread infrastructure is still catching up with demand, and many doctors are still learning about the uses and benefits of proton therapy for prostate cancer. Be sure to talk to your doctor if you haven’t discussed proton radiation as an option for treatment, and don’t be afraid to get a second opinion if your doctor is unfamiliar with proton therapy (UF Health).
Remember that there is no one “right” way to treat prostate cancer, and as with other types of radiation your doctor may order proton therapy in conjunction with other forms of treatment. Other common techniques for treating prostate cancer include surgery, hormone therapy, immunotherapy, cryotherapy, and (in cases where the cancer has spread to other parts of the body) chemotherapy. Only you and your doctor can determine which treatment or combination of treatments is most suitable for you ([2] American Cancer Society).
IN CONCLUSION
Proton therapy is an exciting option for many men who are fighting prostate cancer thanks to its accurate, non-invasive nature. Proton radiation techniques continue to evolve with time, allowing for greater precision, shorter treatment times, and better quality of life during treatment. As proton technology becomes more available in facilities across the U.S., more patients will be able to enjoy its benefits and incorporate proton therapy into an effective battle plan against cancer.
Have Questions About Proton Therapy for Prostate Cancer or Need Help Making Important Treatment Decisions? Contact us, we’re here to help.
RESOURCES
[1] American Cancer Society – Key Statistics for Prostate Cancer.
https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html
Frequently Asked Questions about Proton Therapy. UF Health Proton Therapy Institute.
https://www.floridaproton.org/what-is-proton-therapy/faq
[1] UpToDate.com – Radiation therapy techniques in cancer treatment.
MD Anderson Cancer Center – Proton Therapy for Prostate Cancer.
Journal of Clinical Oncology – Promise and Pitfalls of Heavy-Particle Theapy. Timur Mitin and Anthony L. Zeitman, August 24, 2014.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4152713/
Mayo Clinic – Proton Therapy Risks. Mayo Clinic Staff.
http://www.mayoclinic.org/tests-procedures/proton-therapy/details/risks/cmc-20185458
[2] UpToDate.com. External beam radiation therapy for localized prostate cancer. Steven J DiBiase, MD and Mack Roach III, MD. Topic last updated: April 10, 2017.
[1] UpToDate.com – Radiation therapy techniques in cancer treatment.
[2] American Cancer Society – Treating Prostate Cancer
https://www.cancer.org/cancer/prostate-cancer/treating.html